
World Health Organization (WHO) defines obesity as a body mass index (BMI) of more than two standard deviations above the WHO Growth Reference median for children aged 5 to 19 years.1 Paediatric obesity is a growing global concern, with projections estimating that 18% of girls and 20% of boys worldwide will be obese by 2035.2
Obesity is a multifactorial metabolic disorder highly associated with dietary habits, sedentary lifestyle and socioeconomic status.3 Children who are obese may be predisposed to a significantly higher risk of premature death and disability in adulthood, largely due to the long-term development of chronic conditions such as cardiovascular disease, type 2 diabetes, musculoskeletal disorders, and certain types of cancer.1 Hence, treating obesity early in life is key to improving future health outcomes.
Treating obesity early for better long-term health
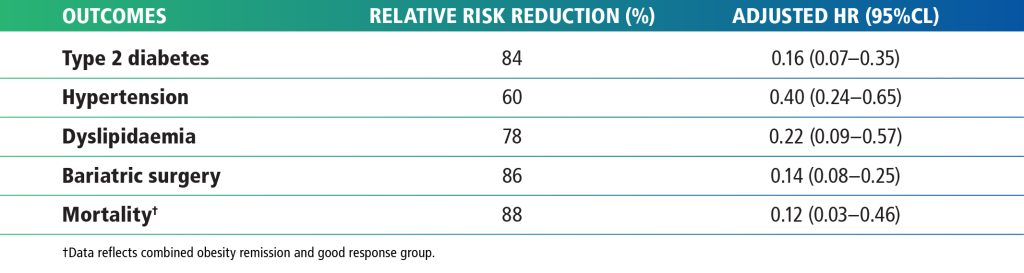
A dynamic prospective cohort study studied participants age 6 to 17 with obesity within the Swedish Childhood Obesity Treatment Register (BORIS) (N = 6,713). The study aimed to evaluate the long-term effects to paediatric obesity treatment on the following critical health outcomes in adulthood over a median treatment duration of 3 years: type 2 diabetes, hypertension, dyslipidaemia, bariatric surgery, and mortality.4
Table 1 shows the outcomes for individuals in the obesity remission group, compared with those in the poor response group. Those who achieved obesity remission had a significantly lower risk of developing type 2 diabetes, hypertension, dyslipidaemia, undergoing bariatric surgery, and mortality compared to the poor response group, indicating that initiating obesity treatment during childhood was associated with reduced long-term morbidity and a lower risk of mortality in young adulthood.4
Table 1: Relative risk of obesity remission group compared to poor response group4
Management of childhood obesity
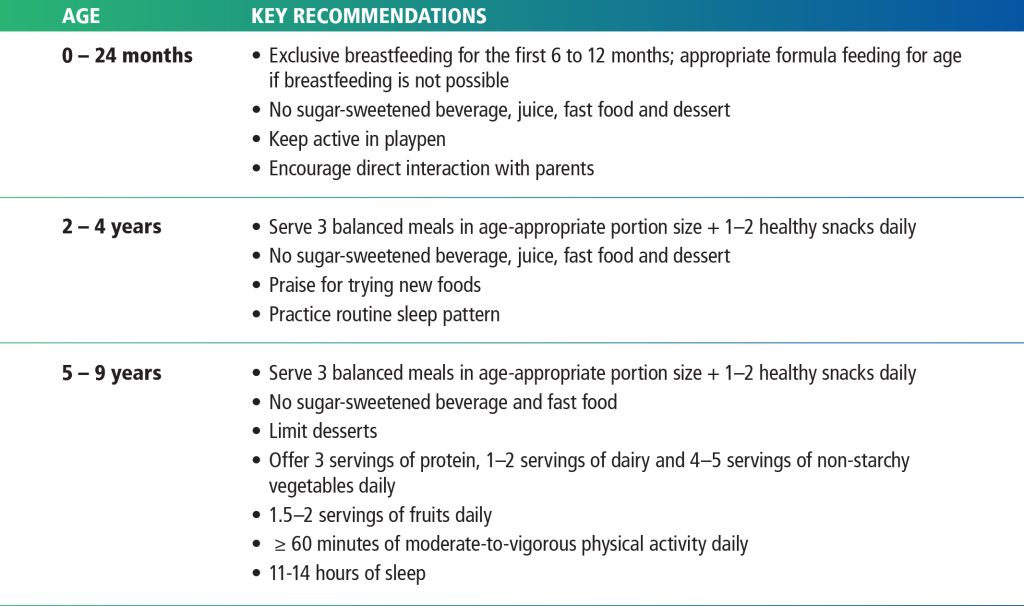
Childhood obesity can be managed with early behavioural and lifestyle interventions, with evidence showing benefits for both immediate and long-term health outcomes.4 Table 2 outlines recommendations for managing childhood obesity in infants and children aged 0 to 9 years old.
Table 2: Management of obesity in different age groups5
Summary
Childhood obesity is far more than a matter of weight; it’s a major public health concern with long-term health consequences. Evidence shows that timely intervention not only improves immediate health but also significantly reduces the risk of chronic diseases in adulthood. By taking early action, we can support healthy growth in children and reduce the burden of non-communicable diseases in the future.
Like what you read?
Let us know what you think.
Contact us for any comments and enquiries:
E: info@mediconnexionsconsulting.com
T: +603 7832 0188
Mediconnexions Consulting Sdn. Bhd. offers a wide range of integrated marketing and communications services related to the medical, pharmaceutical and nutritional sciences.
Visit our website at www.mediconnexionsconsulting.com
Medical webinar organiser Malaysia, creative agency for medical Malaysia, medical conference organiser, medical digital marketing agency, medical marketing agency, medical writer Malaysia, medical writer.
References